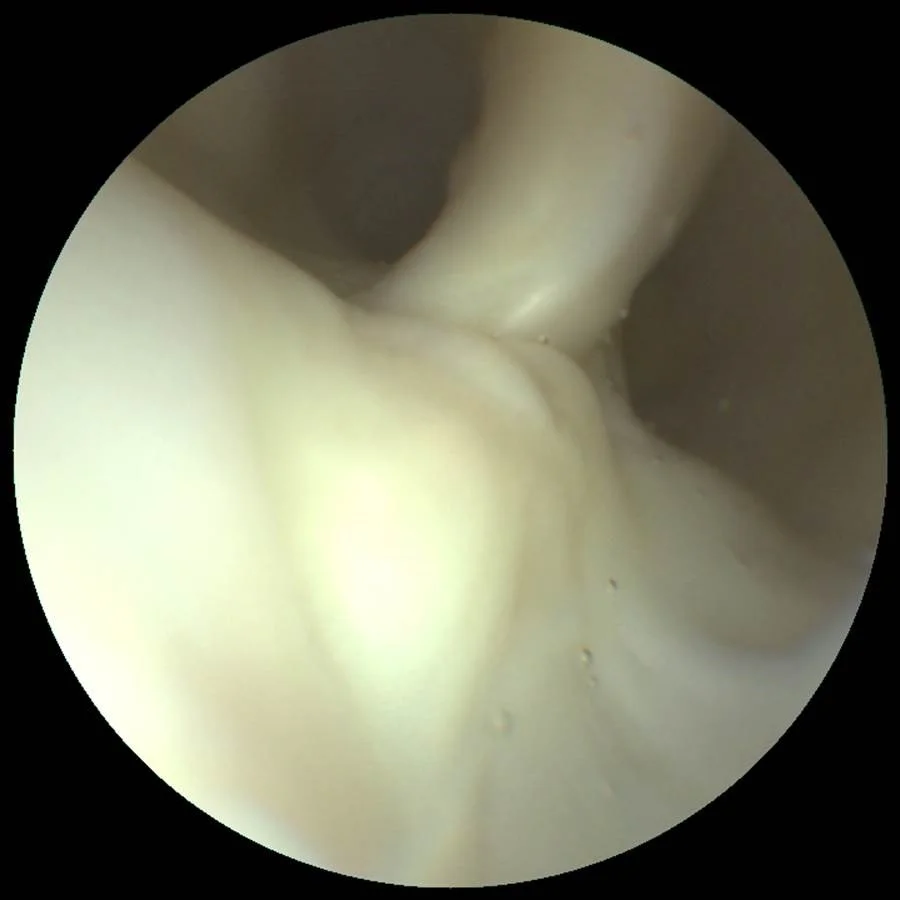
Consider the work that Luis Savastano, MD, is doing in the Department of Neurosurgery, at the University of Michigan Medicine. Dr. Savastano is a physician-scientist specialized in neurosurgery and endovascular neuroradiology. He is pioneering the use of Scanning Fiber Endoscopy (SFE) to detect hallmarks of atherosclerotic plaque rupture and vulnerability. Dr. Savastano summarizes what he has discovered this way, “The SFE can go inside the vessels and snap pictures of the carotid arteries at a very high resolution and find ‘smoking gun’ lesions, such as ruptured plaques, in patients with strokes of unknown cause. In addition, we believe the SFE may even be able to show which silent, but at-risk, plaques may cause a cardiovascular event in the future.”
His groundbreaking work, recently published in two articles in the highly respected journal Nature Biomedical Engineering, introduces SFE as a powerful multimodal platform for atherosclerosis imaging and uncovers the game changer potential for patients suspected to have ruptured but “undetectable” carotid plaques. Dr. Savastano explains, “Many times we may have a suspicion of what happens: the patient has a ruptured atherosclerotic plaque in the carotid artery (one of the most common known reasons of stroke), and it is forming clots that break and travel upstream, occluding vessels in the brain. However, seeing ‘smoking gun’ lesions in the arteries is difficult using available technologies. The majority of tools provide great pictures of the vascular lumen but have many limitations when uncovering subtle thrombogenic lesions (such as shallow ulcers and erosions) in the arterial surfaces, and consequently, many culprit plaques are wrongly labeled as innocent bystanders.” This work, supported by NIH and the Congress of Neurological Surgeons, was distinguished with the Galbraith Award for the top cerebrovascular work by the Americal Association of Neurological Surgeons.
Dr. Savastano’s team has analyzed human cadaveric and surgical tissue and found that patients suffering from cryptogenic stroke actually harbor ruptured lesions in carotid plaques that can originate clots leading to strokes. These lesions may not be detected by the imaging tools currently available, leading to misdiagnosed “cryptogenic" strokes.” These findings were presented this year at the International Stroke Conference and published in Stroke, the flagship journal of the AHA. Dr. Savastano says, “Such miss-diagnoses preclude patients from appropriate and targeted treatment, which translates into unnecessary and unrevealing tests, and a loss of opportunities to prevent future strokes.” He adds, “Angioscopy could be safely performed during workup for cryptogenic stroke, leading to the detection of the root cause of these events. Precise and timely diagnosis of a culprit carotid lesion would provide peace of mind to patients and physicians, strengthen adherence to prescribed treatments, avoid other invasive diagnostic tests (such as brain biopsies and implantable cardiac loop recorders), improve risk stratification of stroke recurrences, and provide a target for medical or surgical interventions leading to reduction of recurrence.”
If successful, Dr. Savastano believes this could ultimately change the standard of care, “Technology like the SFE will be a game-changer in the way we diagnose and treat stroke. The ability to see smoking gun lesions will enable physicians to target the management of ruptured plaques, and likely save more lives or reduce disability, all without undergoing expensive clinical workups.”
Dr. Savastano also believes that SFE provides an opportunity to potentially shift the treatment approach of atherosclerosis, the #1 killer in America, to treatments similar to breast or prostate cancer screening. He explains, “The ability of SFE to identify and monitor the biological markers that render a plaque unstable and at risk for rupture could enable the detection of individuals within high-risk populations who are most likely to suffer from cardiovascular events, and therefore benefit the most from preventive treatment during the asymptomatic stage.” He continues, “In the future, patients with significant cardiac risk factors, such as a family history of heart attacks or smokers, could have their arteries checked with the SFE, and undergo local treatment (such as stenting) if a silent but high-risk plaque is found. In addition, plaque-specific data could help physicians modulate treatment intensity of atherosclerosis, which is currently based on systemic surrogates such as cholesterol and blood sugar levels and occurrence of cardiovascular events such as stroke or myocardial infarction.”